In order to understand how odontogenic infections are treated, the dentist must be familiar with the terminology concerning infection and the pathophysiology of inflammation, which are described below.
Inoculation
is characterized by the entry of pathogenic microbes into the body without disease occurring.An infection involves the proliferation of microbes resulting in triggering of the defense mechanism, a process manifesting as inflammation.
Inflammation
is the localized reaction of vascularand connective tissue of the body to an irritant, resulting in the development of an exudate rich in proteins and cells. This reaction is protective and aims at limiting or eliminating the irritant with various procedures while the mechanism of tissue repair is triggered. Depending on the duration and severity, inflammation is distinguished as acute, subacute or chronic.
Acute Inflammation
This is characterized by rapid progression and is associated with typical signs and symptoms. If it does not regress completely, it may become subacute or chronic.
Subacute Inflammation
This is considered a transition phase between acute and chronic inflammation.
Chronic Inflammation
This procedure presents a prolonged time frame with slight clinical symptoms and is characterized mainly by the development of connective tissue. Inflammation may be caused by, among other things, microbes, physical and chemical factors, heat, and irradiation. Regardless of the type of irritant and the location of the defect, the manifestation of inflammation is typical and is characterized by the following clinical signs and symptoms: rubor (redness), calor (heat), tumor (swelling or edema), dolor (pain), and functio laesa (loss of function).
The natural progression of inflammation is distinguished into various phases. Initially vascular reactions
with exudate are observed (serous phase), and then the cellular factors are triggered (exudative or cellular phase). The inflammation finally resolves and the destroyed tissues are repaired. On the other hand, chronic inflammation is characterized by factors of reparation and healing. Therefore, while acute inflammation is exudative, chronic inflammation is productive (exudative and reparative). Understanding the differences between these types of inflammation is important for therapeutic treatment. Serous Phase. This is a procedure that lasts approximately 36 h, and is characterized by local inflammatory edema, hyperemia or redness with elevated temperature, and pain. Serous exudate is observed at this stage, which contains proteins and rarely polymorphonuclear leukocytes.
Cellular Phase.
This is the progression of the serous phase. It is characterized by massive accumulation of polymorphonuclear leukocytes, especially neutrophil granulocytes, leading to pus formation. If pus forms in a newly developed cavity, it is called an abscess. If it develops in a cavity that already exists, e.g., the maxillary sinus, it is called an empyema.
Reparative Phase
During inflammation, the reparative phenomena begin almost immediately after inoculation. With the reparative mechanism of inflammation, the products of the acute inflammatory reaction are removed and reparation of the destroyed tissues follows. Repair is achieved with development of granulation tissue, which is converted to fibrous connective tissue, whose development ensures the return of the region to normal.
Infections of the Orofacial Region
The majority (i.e., 90–95%) of infections that manifest in the orofacial region are odontogenic. Of these, approximately 70% present as periapical inflammation, principally the acute dentoalveolar abscess, with the periodontal abscess following, etc.
Periodontal abscess originating from a maxillary central incisor.
Radiograph of same case showing bone resorption, which led to the formation of a periodontal pocket
Etiology
The cardinal causes of orofacial infections are non-vital teeth, pericoronitis (due to a semi-impacted mandibular tooth), tooth extractions, periapical granulomas that cannot be treated, and infected cysts. Rarer causes include postoperative trauma, defects due to fracture, salivary gland or lymph node lesions, and infection as a result of local anesthesia.
Periodontal Abscess
This is an acute or chronic purulent inflammation, which develops in an existing periodontal pocket. Clinically, it is characterized by edema located at the middle of the tooth, pain, and redness of the gingiva. These symptoms are not as severe as those observed in the acute dentoalveolar abscess, which is described below.
Treatment of the periodontal abscess is usually simple and entails incision, through the gingival sulcus with a probe or scalpel, of the periodontal pocket that has become obstructed. Incision may also be performed at the gingivae; more specifically, at the most bulging point of the swelling or where fluctuation is greatest.
Acute Dentoalveolar Abscess
This is an acute purulent inflammation of the periapical tissues, presenting at nonvital teeth, especially when microbes exit the infected root canals into periapical tissues. Clinically, it is characterized by symptoms that are classified as local and systemic.
Local Symptoms
Pain
The severity of the pain depends on the stage of development of the inflammation. In the initial phase the pain is dull and continuous and worsens during percussion of the responsible tooth or when it comes into contact with antagonist teeth. If the pain is very severe and pulsates, it means that the accumulation of pus is still within the bone or underneath the periosteum. Relief of pain begins as soon as the pus perforates the periosteum and exits into the soft tissues.
Edema
Edema appears intraorally or extraorally and it usually has a buccal localization and more rarely palatal or lingual. In the initial phase soft swelling of the soft tissues of the affected side is observed, due to the reflex neuroregulating reaction of the tissues, especially of the periosteum. This swelling presents before suppuration, particularly in areas with loose tissue, such as the sublingual region, lips, or eyelids. Usually the edema is soft with redness of the skin. During the final stages, the swelling fluctuates, especially at the mucosa of the oral cavity. This stage is considered the most suitable for incision and drainage of the abscess.
Other Symptoms
There is a sense of elongation of the responsible tooth and slight mobility; the tooth feels extremely sensitive to touch, while difficulty in swallowing is also observed.
Systemic Symptoms
The systemic symptoms usually observed are: fever, which may rise to 39–40 °C, chills,malaise with pain inmuscles and joints, anorexia, insomnia, nausea, and vomiting. The laboratory tests show leukocytosis or rarely leukopenia, an increased erythrocyte sedimentation rate, and a raised C-reactive protein (CRP) level.
Complications
If the inflammation is not treated promptly, the following complications may occur: trismus, lymphadenitis at the respective lymph nodes, osteomyelitis, bacteremia, and septicemia.
Diagnosis
Diagnosis is usually based upon clinical examination and the patient’s history. What mainly matters, especially in the initial stages, is the localization of the responsible tooth. In the initial phase of inflammation, there is soft swelling of the soft tissues. The tooth is also sensitive during palpation of the apical area and during percussion with an instrument, while the tooth is hypermobile and there is a sense of elongation. In more advanced stages, the pain is exceptionally severe, even after the slightest contact with the tooth surface. Tooth reaction during a test with an electric vitalometer is negative; however, sometimes it appears positive,which is due to conductivity of the fluid inside the root canal.
Radiographically, in the acute phase, no signs are observed at the bone (whichmay beobserved 8–10 days later), unless there is recurrence of a chronic abscess,where upon osteolysis is observed. Radiographic verification of a deeply carious tooth or restoration very close to the pulp, as well as thickening of the periodontal ligament, are data that indicate the causative tooth.
Differential diagnosis of the acute dentoalveolar abscess includes the periodontal abscess, and the dentist must be certain of his or her diagnosis, because treatment between the two differs.
Spread of Pus Inside
Tissues From the site of the initial lesion, inflammation may spread in three ways:
1. By continuity through tissue spaces and planes.
2. By way of the lymphatic system.
3. By way of blood circulation.
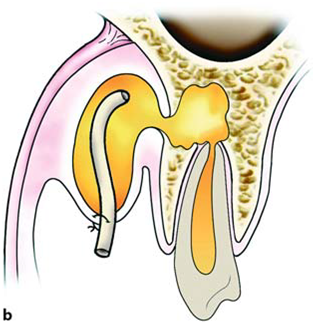
Diagrammatic illustrations showing spread of infection (propagation of pus) of an acute dentoalveolar abscess,depending on the position of the apex of the responsible tooth. a Buccal root: buccal direction.b Palatal root: palatal direction
The most common route of spread of inflammation is by continuity through tissue spaces and planes and usually occurs as described below. First of all, pus is formed in the cancellous bone, and spreads in various directions by way of the tissues presenting the least resistance.
a Spread of pus towards the maxillary sinus, due to the closeness of the apices to the floor of the antrum.b Diagrammatic illustration showing the localization of infection above or below the mylohyoid muscle, depending on the position of the apices of the responsible tooth
Whether the pus spreads buccally, palatally or lingually depends mainly on the position of the tooth in the dental arch, the thickness of the bone, and the distance it must travel.Purulent inflammation that is associated with apices near the buccal or labial alveolar bone usually spreads buccally, while that associated with apices near the palatal or lingual alveolar bone spreads palatally or lingually respectively. For example,the palatal roots of the posterior teeth and the maxillary lateral incisor are considered responsible for the palatal spread of pus, while the mandibular third molar and sometimes the mandibular second molar are considered responsible for the lingual spread of infection. Inflammation may even spread into the maxillary sinus when the apices of posterior teeth are found inside or close to the floor of the antrum. The length of the root and the relationship between the apex and the proximal and distal attachments of various muscles also play a significant role in the spread of pus. Depending on these relationships, in the mandible pus originates from the apices found above themylohyoid muscle, and usually spreads intraorally, mainly towards the floor of the mouth (sublingual space). When the apices are found beneath the mylohyoid muscle (second and third molar), the pus spreads towards the submandibular space, resulting in extraoral localization. Infection originating from incisors and canines of the mandible spreads buccally or lingually, due to the thin alveolar bone of the area. It is usually localized buccally if the apices are found above the attachment of the mentalis muscle. Sometimes, though, the pus spreads extraorally, when the apices are found beneath the attachment. In the maxilla, the attachment of the buccinators muscle is significant.When the apices of the maxillary premolars and molars are found beneath the attachment of the buccinator muscle, the pus spreads intraorally; however, if the apices are found above its attachment, infection spreads upwards and extraorally. Exactly the same phenomenon is observed in the mandible as in the maxilla if the apices are found above or below the attachment of the buccinator muscle.


Spread of pus depending on the length of root and attachment of buccinators muscle. a Apex above attachment: accumulation of pus in the buccal space. b Apex beneath the buccinator muscle: intraoral pathway towards the mucobuccal fold
In the cellular stage, depending on the pathway and inoculation site of the pus, the acute dentoalveolar abscessmay have various clinical presentations, such as:(1) intraalveolar, (2) subperiosteal, (3) submucosal, (4) subcutaneous, and (5) fascial ormigratory – cervicofacial.
Intraalveolar abscess of maxilla (a) and mandible (b). Diagrammatic illustrations show accumulation of pus at a portion of the alveolar bone in relation to the periapical region
The initial stage of the cellular phase is characterized by accumulation of pus in the alveolar bone and is termed an intraalveolar abscess . The pus spreads outwards from this site and, after perforating the bone, spreads to the subperiosteal space, from which the subperiosteal abscess originates, where a limited amount of pus accumulates between the bone and periosteum. After perforation of theperiosteum, the pus continues to spread through the soft tissues in various directions. It usually spreads intraorally, spreading underneath the mucosa forming the submucosal abscess.
Subperiosteal abscess with lingual localization. a Diagrammatic illustration; b clinical photograph
Sometimes, though,it spreads through the loose connective tissue and, after its pathway underneath the skin, forms a subcutaneous abscess, while other times it spreads towards the fascial spaces, forming serious abscesses called fascial space abscesses.
Subcutaneous abscess originating from a mandibular tooth. a Diagrammatic illustration. b Clinical photograph.The swelling mainly involves the region of the angle of the mandible
The fascial spaces are bounded by the fascia, which may stretch or be perforated by the purulent exudate, facilitating the spread of infection. These spaces are potential areas and do not exist in healthy individuals, developing only in cases of spread of infection that have not been treated promptly. Some of these spaces contain loose connective tissue, fatty tissue, and salivary glands,while others contain neurovascular structures. Acute diffuse infection,which spreads into the loose connective tissue to agreat extent underneath the skin with or without suppuration,is termed “cellulitis” (phlegmon), and is described in next posts.
Fascial abscess (submandibular). a Diagrammatic illustration. b Clinical photograph
Next Post : Fundamental principles of treatment of infection
Tags : Odontogenic infections, Infections of Oromaxillofacial Region, Infection from lower 3rd molar,Spread of infections,Factors determining spread of infections,Spread of Infections.
Key Words : oral surgeons wisdom teeth extraction dental implant surgery doctor of dental surgery oral surgeon dental operation dental gum surgery wisdom tooth surgery dental surgery oral surgery doctor of dental surgery cosmetic dental surgery dental laser surgery cosmetic gum surgery laser gum surgery