1. Impression compound
2. Impression Plaster
3. Zinc Oxide Eugenol
4. Impression Waxes
Impression Plaster
The plaster should be mixed with water or an anti-expansion solution in the ratio of 100g to 50-60ml. The mix should be a smooth paste, free of air bubbles, which may appear on the surface of the impression leading to inaccuracy. The tray should be loaded and "puddled" into position, and held in place until set. As the impression is removed from the mouth it is not uncommon for pieces of plaster around the periphery of the impression to fracture off. These pieces should be retrieved and glued back onto the impression before it is cast. Long narrow strips of wax are then fit around the periphery of the impression just below where it ends. This is called beading. The impression is then coated with a thin layer of separating medium and cast in fresh plaster. The beading provides a clear indication of where the impression ends; the creation of this level area prevents over-trimming and over-extension.
Properties of Impression Plaster
CHEMISTRY
Impression plaster is based on calcined (להישרף) calcium sulphate hemihydrate, which reacts with water to form a hard mass of calcium sulphate dihydrate.
This setting reaction is associated with an expansion of 0.3-0.6%. When this is within the confines of an impression tray it will lead to a significant reduction in accuracy.
Mixing the plaster with anti-expansion solution (containing 4% potassium sulphate and 0.4% borax) will reduce this. The potassium sulphate reduces expansion to 0.05%, but this also accelerates the setting reaction, and borax is added as a retarder, which gives more time to take the impression.
PROPERTIES
- Excellent at recording fine detail (because very fluid when inserted in mouth)
- Dimensionally stable if anti expansion solution used
- Fractures if undercuts present
- Mucostatic
- Needs to be treated with a separating medium (e.g. varnish or soap solution) before being cast in stone or plaster
- Exothermic setting reaction
- On storage dimensionally stable but a small amount of shrinkage may occur
- Non toxic but may be unpleasant due to dryness and heat evolved during setting
ADVANTAGES
- Good surface detail
- Excellent dimensional stability
- Rate of the setting reaction can be controlled by the clinician
DISADVANTAGES
- Cannot be used for mucocdisplacive impressions
- Cannot be added to
- Properties affected by operator handling technique
- Taste and roughness may cause the patient to vomit
Impression Compound
The compound disc is completely immersed in a water bath at 55-60oC for about 4-5 minutes to ensure complete softening. Gauze is placed at the bottom of the water bath to prevent adherence. However if it is left in too long some of the constituents may be leached out into the water bath, altering the properties of the material (it is often the plasticiser stearic acid that is leached out). If the compound is kneaded water will become incorporated and act as a plasticiser. The compound is loaded on to the tray and firm pressure is used to seat the tray home in the mouth. After the impression has been taken it is carefully examined, a common mistake is not softening the compound enough. In this is the case the impression can be reheated in a separate bowl of water (cross infection control) and the impression is repeated.
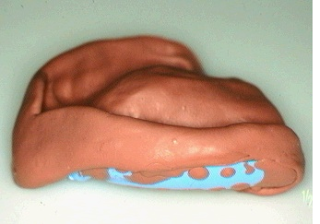
| 1) An impression compound disc | 2) An impression compound impression taken in an upper edentulous stock tray |
Properties of Impression Compound
CHEMISTRY
Made up of 3 constituents
1. Resins (e.g. wax)
2. Filler (e.g. talc or soapstone)
3. Lubricants (stearic acid or stearin)
It is a thermoplastic compound i.e. it softens when heated and hardens when cooled. This process does not involve a chemical reaction.
Impression compound is available in 2 forms:
1. Stick form - used for modifying impression trays. Softening temperature is 700C
2. Sheet form - used to take impressions of the mouth. Softening temp is 55-600C.
PROPERTIES
- Poor surface detail
- High coefficient of thermal expansion (contraction of up to 0.3% when removed from mouth to room temperature)
- Distorts when removed over undercut areas
- Mucocodisplacive
- Poor dimensional stability
- Can be modified by re-heating
- Non toxic and non irritant
- Good shelf life
ADVANTAGES
1. Non irritant and non toxic
2. Reusable (but with re-use the constituents are leached out)
3. Can be reheated and readapted
4. Can support other materials for wash impressions
5. Mucocompressive
DISADVANTAGES
1. Poor dimensional stability
2. Poor surface detail
3. Expansion coefficient
4. Will distort if removed from undercuts
Impression Waxes
Waxes are thermoplastic materials, which flow at mouth temperature and are soft a room temperature. They do not set by chemical reaction. Normally used to correct small imperfection (e.g. airblows) in other impressions, especial zinc oxide impressions. They consist of a combination of a low melting paraffin wax and beeswax in a ratio of approximately 3:1 to ensure the wax flows at room temperature. A cast should be poured up immediately after taking the impression to avoid distortion which readily occurs in wax. These materials are not commonly used.
Zinc Oxide-Eugenol
Impression Material
This material is used for recording edentulous ridges in a close fitting special tray or the patients existing dentures. The material is mixed in a 1:1 paste ratio and used in thin sections only (2-3mm) as a wash impression. Vaseline is used as a separating agent on those areas requiring protection (soft tissues, teeth etc). Firm pressure is used during impression taking.
Properties of Zinc-Oxide Eugenol
CHEMISTRY
Constituents of a typical zinc oxide eugenol paste are:
BASE PASTE
- Zinc oxide
- Inert oils (plasticiser)
- Hydrogenated resins (increases setting time and improves cohesion)
REACTOR PASTE
- Eugenol
- Zinc acetate (accelerator)
- Fillers (talc or kaolin)
Some pastes contain a substitute for eugenol e.g. a carboxylic acid.
The 2 pastes come in contrasting colours and are dispensed in a 1:1 ratio. They are mixed to give a paste of even colour. The setting reaction is shown below:
| ZINC OXIDE (excess) | ZINC OXIDE (UNREACTED) |
| + | -> + |
| EUGENOL | EUGENOL |
The set material contains both some unreacted zinc oxide and eugenol.
Any movement of the tray as the paste is hardening will lead to a deformed, inaccurate impression.
Setting time depends on:
1. Accelerator additives (e.g. zinc acetate, acetic acid)
2. Exposure to moisture on mixing or the addition of water will accelerate the reaction
3. Increasing temperature causes a faster setting reaction
Setting time is normally 4-5 minutes.
PROPERTIES
- Non toxic
- Adherence to tissues
- Mucostatic or mucocodisplacive (depending on brand used)
- Good surface detail in thin section
- Good dimensional stability (little or no dimensional change on setting, 0.1% dimensional change during setting)
- Can be added to with fresh zinc oxide eugenol
- Stable on storage and good shelf life
ADVANTAGES
1. Dimensional stability
2. Good surface detail
3. Can be added to
4. Mucostatic or mucocodisplacive
DISADVANTAGES
1. Cannot be used in very deep undercuts
2. Only sets quickly in thin section
3. Eugenol allergy in some patients