A conventional over-denture rests over some healthy natural tooth roots.
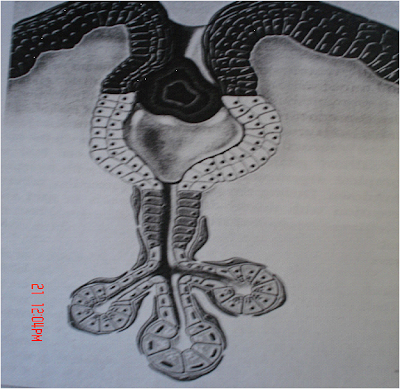
An overview of the Jaw
Maintaining a denture on the jaw bone ridge (called alveolar ridge) is essential to preventing it from becoming loose during eating, speaking and other activities.
Preserving the alveolar ridge facilitates denture stability
The body tends to conserve energy and nutrients by maintaining only structures with apparent immediate value. A typical example is the bulk reduction of a broken leg held immobile by a full leg cast for a month or more.
The body "recognizes" the only one purpose for alveolar bone is to hold tooth roots.
Alveolar bone no longer supporting a tooth root is removed, or literally dissolved away by the body. This is called resorption or simply shrinkage.
Resorption progresses at varying rates in the same person at different times and at different rates between different people. Resorption progresses rapidly within the first year of loosing a tooth after which time the rate progresses at a slower pace.
Preserving the Jaw bone
IF the maximum amount of bone is to be maintained then preserving the maximum number of healthy tooth roots should achieve that end.
Preserving the sensation of having teeth
Studies demonstrate that even though only roots are preserved, and they are covered by a denture, a patient still has sensory input sensations similar to that experienced with teeth, as opposed to individuals with conventional dentures and no preserved roots. Over-denture patients also appear to have a more natural perceived directional sense in their chewing activities. In other words, many patients relate that they still feel like they have teeth - - a positive comment.
Why an over-denture?
If a patient is treatment planned to have a denture, and the roots of some remaining teeth are supported in healthy alveolar bone - - then a conventional over-denture is a viable consideration.
However, only a licensed dental professional can determine if a conventional over-denture is a suitable consideration for a certain person, after a comprehensive examination.
Some characteristics of a conventional over-denture
- Most of a tooth crown (that part of the tooth above the gums) is removed. This often necessitates root canal therapy if not already done.
- Remaining tooth, projecting above the gum, is rounded and usually covered with a similarly shaped artificial crown-like covering.
- Various configurations and extensions may be built onto some retained roots. In those cases, that portion of the denture overlying these configurations is modified to contain attachments that clip onto a framework or receive the individual extensions. In addition to preserving alveolar bone and sensory input, the denture is securely held in place, but may be comfortably and easily removed for cleaning.
Advantages of a conventional over-denture
- Feels more like having teeth
- More retentive in many cases
- Helps reduce shrinkage of surrounding bone
- Reduces pressure to portions of the alveolar ridge
- Positive psychological advantage of still having teeth
Disadvantages of a conventional over-denture
- Scrupulous oral hygiene is essential in order prevent decay and gum disease.
- The over-denture may feel bulkier than a conventional denture.
- Frequent maintenance examinations are necessary.
- Generally this is a more expensive approach than a conventional denture.
Implant Over-Denture
An implant over-denture connects to cylinder-like configurations (called implants) that have been surgically implanted into jaw bone.
The denture appears like a traditional prosthesis. However, that part of the denture overlying implants is modified to retain various semi-rigid attachments that receive implant extensions projecting above the gum. This arrangement helps keep a denture securely in place while eating, speaking and during other oral activities, but still allows easy self-removal of the denture for cleaning purposes.
There are two phases to this process. The first is a surgical phase consisting of two stages, and the second is a prosthetic phase (making the implant denture).
The surgical phase
Surgical insertion stage
Implants are completely inserted into precise preparations in jaw bone. While there are various implant configurations, they are essentially cylindrical in shape and made of pure titanium metal. After implants are inserted into jaw bone, gum tissue over the implant is closed with sutures in most cases.
While a minimum of two implants may be inserted for an acceptable outcome, a person may be treatment planned to receive three or more - - depending upon individual needs and anatomical limitations. More implants will give additional support and retention to the implant denture.
Healing and surgical exposure stage
During healing, an existing or temporary denture may continue to be worn after adjustments have been made to adapt to the surgerized site. If the existing denture cannot be altered sufficiently, a provisional prosthesis should be fabricated.
Implants are left undisturbed beneath gum tissue for at least several months as determined by the dental professional. During this time bone reorganizes and grows around the implant surface, anchoring it securely into the jaw (this is called osseointegration).
At the end of the healing stage, the top of the implant is exposed by removing gum tissue directly over it.
An extension that is then screwed into the exposed implant projects slightly above the gum tissue. After adjustments, an existing denture can be worn over an implant extension while the gum heals.
However, the denture must be reshaped to conform to surgical site contours in order to avoid unnecessary pressure areas on the newly surgerized site.
The prosthetic phase (making the implant denture)
A precision superstructure is fabricated that is screwed into the implant extensions. This superstructure may have various interface configurations ranging from interconnecting metal bars to specially shaped singular extensions.
A denture is fabricated with special provisions on the inside surface to receive various types of attachments (interlocks). Depending on the attachment, they interact in various ways with the superstructure. For example, a metal or plastic attachment may clip onto metal superstructure bars, a nylon receptacle may receive a specially configured implant extension, and so forth.
The attachment/superstructure configuration helps to securely maintain a denture while eating and speaking, and still allows a person to comfortably and easily remove the prosthesis for cleaning purposes.
Essential maintenance needs
As might be expected, exemplary oral hygiene is essential to helping prevent the development of disease around implants that could cause their failure.
Implants, superstructure, attachments and the over-denture must be checked and professionally maintained by a licensed dental professional on a regular basis. Attachments often need periodic adjustment or replacement due to wear.
While the implant over-denture approach is complex and expensive, the value received by an individual usually far exceeds monetary considerations.
How long will implant over-dentures last?
An implant may last for a lifetime (current reports show many implants lasting twenty years) or deteriorate in a few years - many factors are involved that reduce the life expectancy of implants, such as oral hygiene, general health, habits such as smoking, grinding, and so forth. The superstructure or implant extensions may need to be replaced after five years. Depending on the implant system used, some parts may need to be replaced annually, or sooner, because of wear or deterioration. These time frames are generalities. The dental profession continues to strive for long-term durability.