Dental Caries Definition:
“Dental caries is an irreversible microbial disease of the calcified tissues of the teeth, charecterized by demineralization of the inorganic portion and destruction of the organic substance of the tooth , which often leads to cavitation”
Dental caries are classified based on following factors.
1. Based on anatomical site
2. Based on progression
3. Based on virginity of lesion
4. Based on extend of caries
5. Based on tissue involvement
6. Based on pathway of caries spread
7. Based on number of tooth surface involved
8. Based on chronology
9. Based on whether caries is completely removed or not during treatment
10. Based on tooth surface to be restored
11. Black’s classification
12. WHO system
Dental caries-Classification based on Anatomical Site
- Occlusal (Pit and Fissure caries)
- Smooth surface caries (Proximal and cervical caries)
- Linear enamel caries
- Root caries
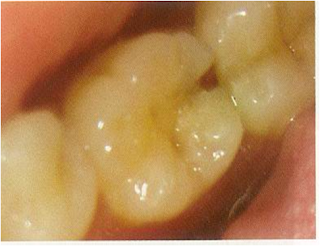
Pit and Fissure caries
- Highest prevalence of all caries bacteria rapidly colonize the pits and fissures of the newly erupted teeth
- These early colonizers form a “bacterial plug” that remains in the site for long time ,perhaps even the life of the tooth
- Type & nature of the organisms prevalent in the oral cavity determine the type of organisms colonizing the pit & fissure
- Numerous gram positive cocci, especially dominated by s.sanguis are found in the newly erupted teeth.
- The appearance of s.mutans in pits and fissures is usually followed by caries 6 to 24 months later (Window Period).
- Sealing of pits and fissures just after tooth eruption may be the most important event in their resistance to caries.
- Shape, morphological variation and depth of pit and fissures contributes to their high susceptibility to caries.
- Caries expand as it penetrates in to the enamel.
Morphology of Fissures
NANGO (1960): Based on the alphabetical description of shape– 4 types
V&U type: self cleansing and somewhat caries resistant
U type: narrow slit like opening with a larger base as it extend towards DEJ .Caries susceptible; also have a number of different branches
K type: also very susceptible to caries
- Entry site may appear much smaller than actual lesion, making clinical diagnosis difficult.
- Carious lesion of pits and fissures develop from attack on their walls.
- In cross section, the gross appearance of pit and fissure lesion is inverted V with a narrow entrance and a progressively wider area of involvement closer to the DEJ.
Smooth surface caries
- Less favorable site for plaque attachment, usually attaches on the smooth surface that are near the gingiva or are under proximal contact.
- In very young patients the gingival papilla completely fills the interproximal space under a proximal contact and is termed as col. Also crevicular spaces in them are less favorable habitats for s.mutans.
- Consequently proximal caries is less lightly to develop where this favorable soft tissue architecture exists.
- The proximal surfaces are particularly susceptible to caries due to extra shelter provided to resident plaque owing to the proximal contact area immediately occlusal to plaque.
- Lesion have a broad area of origin and a conical, or pointed extension towards DEJ.
- V shape with apex directed towards DEJ.
- After caries penetrate the DEJ softening of dentin spread rapidly and pulpally
 |
| Smooth surface caries Radiograph |
Linear enamel caries
- Linear enamel caries (odontoclasia) is seen to occur in the region of the neonatal line of the maxillary anterior teeth.
- The line, which represents a metabolic defect such as hypocalcemia or trauma of birth, may predispose to caries, leading to gross destruction of the labial surface of the teeth.
- Morphological aspects of this type of caries are atypical and results in gross destruction of the labial surfaces incisor teeth
Root surface caries
- The proximal root surface, particularly near the cervical line, often is unaffected by the action of hygiene procedures, such as flossing, because it may have concave anatomic surface contours (fluting) and occasional roughness at the termination of the enamel.
- These conditions, when coupled with exposure to the oral environment (as a result of gingival recession), favor the formation of mature, caries-producing plaque and proximal root-surface caries.
- Root-surface caries is more common in older patients.
· Caries originating on the root is alarming because
1. It has a comparatively rapid progression
2. It is often asymptomatic
3. It is closer to the pulp
4, it is more difficult to restore
- The root surface is refer the enamel and readily allows plaque formation in the absence of good oral hygiene.
- The cementum covering the root surface is extremely thin and provides little resistance to caries attack.
- Root caries lesions have less well-defined margins, tend to be U-shaped in cross sections, and progress more rapidly because of the lack of protection from and enamel covering.
 |
| Root Suraface caries-Radiograph |
Dental Caries-Classification based on Progression
- Acute caries
- Chronic caries
- Arrested caries
Acute caries
· Acute caries is a rapid process involving a large number of teeth.
· These lesions are lighter colored than the other types, being light brown or grey, and their caseous consistency makes the excavation difficult.
· Pulp exposures and sensitive teeth are often observed in patients with acute caries.
· It has been suggested that saliva does not easily penetrate the small opening to the carious lesion, so there are little opportunity for buffering or neutralization
Chronic caries
· These lesions are usually of long-standing involvement, affect a fewer number of teeth, and are smaller than acute caries.
· Pain is not a common feature because of protection afforded to the pulp by secondary dentin
· The decalcified dentin is dark brown and leathery.
· Pulp prognosis is hopeful in that the deepest of lesions usually requires only prophylactic capping and protective bases.
· The lesions range in depth and include those that have just penetrated the enamel.
Arrested caries
· Caries which becomes stationary or static and does not show any tendency for further progression
· Both deciduous and permanent affected
· With the shift in the oral conditions, even advanced lesions may become arrested.
· Arrested caries involving dentin shows a marked brown pigmentation and indurations of the lesion [the so called ‘eburnation of dentin’]
· Sclerosis of dentinal tubules and secondary dentin formation commonly occur
· Exclusively seen in caries of occlusal surface with large open cavity in which there is lack of food retention
· Also on the proximal surfaces of tooth in cases in which the adjacent approximating tooth has been extracted
Dental Caries-Classification based on Virginity of the lesion
- Initial/Primary
- Recurrent/Secondary
Primary caries (initial)
· A primary caries is one in which the lesion constitutes the initial attack on the tooth surface.
· The designation of primary is based on the initial location of the lesion on the surface rather than the extent of damage.
Secondary caries (recurrent)
· This type of caries is observed around the edges and under restorations.
· The common locations of secondary caries are the rough or overhanging margin and fracture place in all locations of the mouth.
· It may be result of poor adaptation of a restoration, which allows for a marginal leakage, or it may be due to inadequate extension of the restoration.
· In addition caries may remain if there has not been complete excavation of the original lesion, which later may appear as a residual or recurrent caries.
Dental Caries-Classification based on extent of the caries
- Incipient caries
- Occult caries
- Cavitation
Incipient caries
· The early caries lesion, best seen on the smooth surface of teeth, is visible as a ‘white spot’.
· Histologically the lesion has an apparently intact surface layer overlying subsurface demineralization.
· Significantly may such lesion can undergo remineralization and thus the lesion per se is not an indication for restorative treatment
· These white spot lesion may be confused initially with white developmental defects of enamel formation, which can be differentiated by their position away from the gingival margin], their shape [unrelated to plaque accumulation] and their symmetry [they usually affect the contra lateral tooth].
· Also on wetting the caries lesion disappear while the developmental defect persist
· It is believed that bite wing and OPG radiographs along with noninvasive adjuncts like fiber optic transillumination (FOTI),laser luminescence, electrical resistance method (ERM) are used for diagnosis these occlusal lesions.
· These lesions are not associated with microorganisms different to those found in other carious lesion.
· These carious lesions seem to increase with increasing age.
· Occult carious lesions are usually seen with low caries rate which is suggestive of increase fluid exposure.
· It is believed that increased fluid exposure encourages remineralization and slow down progress of the caries in the pit and fissure enamel while the cavitations continues in dentine, and the lesions become masked by a relatively intact enamel surface.
· These hidden lesions are called as fluoride bombs or fluoride syndrome.
· Recently it is seen that occult caries may have its origin as pre-eruptive defects which are detectable only with the use of radiographs.
· Once it reaches the dentinoenamel junction, the caries process has the potential to spread to the pulp along the dentinal tubules and also spread in lateral direction.
· Thus some amount of sensitivity may be associated with this type of lesion.
· This may be generally accompanied by cavitation
Dental Caries-Classification based on Tissue involvement
- Initial caries
- Superficial caries
- Moderate caries
- Deep caries
- Deep complicated caries
Dental caries can be divided into 4 or 5 stages
1. Initial caries: Demineralization without structural defect. This stage can be reversed by fluoridation and enhanced mouth hygiene
2. Superficial caries (Caries superficialis):Enamel caries, wedge-shaped structural defect. Caries has affected the enamel layer, but has not yet penetrated the dentin.
3. Moderate caries (Caries media): Dentin caries. Extensive structural defect. Caries has penetrated up to the dentin and spreads two-dimensionally beneath the enamel defect where the dentin offers little resistance.
4. Deep caries (Caries profunda): Deep structural defect. Caries has penetrated up to the dentin layers of the tooth close to the pulp.
5. Deep complicated caries (Caries profunda complicata) :Caries has led to the opening of the pulp cavity (pulpa aperta or open pulp).
Dental Caries-Classification based on pathway of caries spread
- Forward caries
- Backward caries
“Forward-backward” classification is considered as graphical representation of the pathway of dental caries.
Enamel
- First component of enamel to be involved in carious process is the interprismatic substance. The disintegrating chemicals will proceed via the substance, causing the enamel prism to be undermined.
- The resultant caries involvement in enamel will have cone shape.
In concave surface (pit and fissures) base towards DEJ.
In convex surfaces (smooth surface) base away from DEJ.
Dentin
· First component to be involved in dentin is protoplasmic extension within the dentinal tubules.
· These protoplasmic extension have their maximum space at the DEJ, but as they approach the pulp chamber and root canal walls, the tubules become more densely arrange with fewer interconnections.
· So caries cone in dentin will have their base towards DEJ.
· Decay starts in enamel then it involves the dentin. Wherever the caries cone in enamel is larger or at least the size as that of dentin, it is called forward decay (pit decay)
· However the carious process in dentin progresses much faster than in enamel, so the cone in dentin tends to spread laterally creating undermined enamel. In addition decay can attack enamel from its dentinal side. At this stage it becomes backward decay.
Dental Caries-Classification based on number of tooth surfaces involved
- Simple-A caries involving only one tooth surface
- Compound-A caries involving two surfaces of tooth
- Complex-A caries that involves more than two surfaces of a tooth
Dental Caries-Classification based on Chronology
- Early childhood caries
- Adolescent caries
- Adult caries
· It has been stated that over a lifetime, caries incidence i.e. the number of new lesions occurring in a year, shows three peaks-at the ages 4-8,11-19 and 55-65 years
Early childhood caries
· Early childhood caries would include two variants: Nursing caries and rampant caries.
· The difference primarily exist in involvement of the teeth [mandibular incisors ] in the carious process in rampant caries as opposed to nursing caries.
Classification of early childhood caries
Type 1 (Mild)
· Involves molars and incisors
· Seen in 2-5 years
· Cause-cariogenic semisolid food +lack of oral hygeine
Type 2 (Moderate)
· Unaffected mandibular incisors
· Soon after first tooth erupts
· Cause-inappropriate feeding +lack of oral hygeine
Type 3 (Severe)
· All teeth including mandibular incisors
· Cause-multitude of factors
Synonyms
Nursing caries, Nursing bottle mouth, Nursing bottle syndrome, Bottle-Propping caries, comforter caries, Baby Bottle mouth, Nursing Mouth Decay, Baby bottle tooth decay, tooth cleaning neglect
New name-Maternally derived streptococcus mutant disease (MDSMD)
NURSING CARIES · toddler - Affects primary dentition
- Mandibular incisors are
not involved Etiology · feeding - Pacifier dipped in honey/other sweetner
| RAMPANT CARIES - Seen in all ages,
- including adoloscennce
- Affects primary and
· permanent dentition also affected Etiology · Multifactorial Frequent snacks Sticky refined CHO Decreased salivary flow Genetic background |
Teenage caries (adolescent caries)
· This type of caries is a variant of rampant caries where the teeth generally considered immune to decay are involved.
· The caries is also described to be of a rapidly burrowing type, with a small enamel opening.
· The presence of a large pulp chamber adds to the woes, causing early pulp involvement
Adult caries
· With the recession of the gingiva and sometimes decreased salivary function due to atrophy, at the age of 55-60 years, the third peak of caries is observed.
· Root caries and cervical caries are more commonly found in this group.
· Sometime they are also associated with a partial denture clasp.
Dental caries Classification based on whether caries is completely removed or not during treatment
Residual caries
· Residual caries is that which is not removed during a restorative procedure, either by accident, neglect or intention.
· Sometimes a small amount of acutely carious dentin close to the pulp is covered with a specific capping material to stimulate dentin deposition, isolating caries from pulp.
· The carious dentin can be removed at a later time.
Dental Caries-Classification based on surfaces to be restored
· Most widespread clinical utilization
O for occlusal surfaces
M for mesial surfaces
D for distal surfaces
F for facial surfaces
B for buccal surfaces
L for lingual surface
Various combinations are also possible, such as MOD –for mesio-occluso-distal surfaces.
Dental Caries-Black’s classification
Class 1 lesions:
· Lesions that begin in the structural defects of teeth such as pits, fissures and defective grooves.
Locations include
· Occlusal surface of molars and premolars.
· occlusal two thirds of buccal and lingual surfaces of molars and premolars.
· Lingual surfaces of anterior tooth.
Class 2 lesions:
· They are found on the proximal surfaces of the bicuspids and molars.
Class 3 lesions:
· Lesions found on the proximal surfaces of anterior teeth that do not involve or necessitate the removal of the incisal angle.
Class 4 lesions:
· Lesions found on the proximal surfaces of anterior teeth that involve the incisal angle.
Class 5 lesions:
· Lesions that are found at the gingival third of the facial and lingual surfaces of anterior and posterior teeth.
Class 6 (Simon’s modification):
· Lesions involving cuspal tips and incisal edges of teeth.
Dental Caries-Classification World Health Organization (WHO) system
In this classification the shape and depth of the caries lesion scored on a four point scale
- D1. Clinically detectable enamel lesions with intact (non cavitated) surfaces
- D2. Clinically detectable cavities limited to enamel
- D3. Clinically detectable cavities in dentin
- D4. Lesions extending into the pulp
Radiation Caries
- Radiography is frequently associated with xerostomia due to decreased salivary secretion,an increase in viscosity and low PH
- This and other causes of decreased salivary secretion may lead to a rampant form of caries, including the significance of saliva in preventing caries.
Three types of defects due to irradiation
- Lesion usually encircling the neck of teeth amputation of crowns may occur
- Begins as brown to black discolouration of tooth .occlusal surface and incisal edges wear away
- Spot depression which spreads from any surface
Classifications of cavity preparations
Based on treatment and restoration design (black’s)
Class 1 restoration:
· include the structural defects of teeth such as pits, fissures and defective grooves.
· Locations include
· Occlusal surface of molars and premolars.
· occlusal two thirds of buccal and lingual surfaces of molars and premolars.
· Lingual surfaces of anterior tooth.
Class 2 restoration:
· They are found on the proximal surfaces of the bicuspids and molars.
Class 3 restoration:
· Restoration on the proximal surfaces of anterior teeth that do not involve or necessitate the removal of the incisal angle.
Class 4 restoration:
· Restoration on the proximal surfaces of anterior teeth that involve the incisal angle.
Class 5 restoration:
· Restoration at the gingival third of the facial and lingual surfaces of anterior and posterior teeth.
Class 6 (Simon’s modification):
· Restoration involving cuspal tips and incisal edges of teeth.
Other Modifications
Charbeneu’s modification:
a) Class 2:-cavity on single proximal surface of bicuspids and molars
b) Class 6:
Cavities on both mesial and distal proximal surfaces of posterior teeth that will share a common occlusal isthmus
c) Lingual surfaces of upper anterior teeth.
d) Any other unusually located pit or fissure involved with decay.
Sturdevant’s classification
Cavity Feature
Simple cavity-A cavity involving only one tooth surface
Compound cavity-A cavity involving two surfaces of tooth
Complex cavity-A cavity that involves more than two surfaces of a tooth
Finn’s modification of Black’s cavity preparation for primary teeth
· Class1: Cavities involving the pits and fissures of molar teeth and the buccal and lingual pits of all teeth.
· Class 2: cavities involving proximal surface of molar teeth will access established from the occlusal surface.
· Class 3: cavities involving proximal surfaces of anterior teeth which may or may not involve a labial or a lingual extension
· Class 4: a restoration of the proximal surface of an anterior tooth which involves the restoration of an incisal angle.
· Class 5: cavities present on the cervical third of all teeth, including proximal surface where the marginal ridge is not included in the cavity preparation
Baume’s classification
a). Pit and fissure cavities
b). Smooth surface cavities
Classification by Mount and Hume (1998)-G.J.Mount classification
· This new system defines the extent and complexity of a cavity and at the same time encourages a conservative approach to the preservation of natural tooth structure.
· This system is designed to utilize the healing capacity of enamel and dentine.
The three sites of carious lesions:
· Site 1-Pits, fissures and enamel defects on occlusal surfaces of posterior teeth or other smooth surfaces
· Site 2-Proximal enamel immediately below areas in contact with adjacent teeth
· Site 3-The cervical one third of the crown or following gingival recession, the exposed root
The four sizes of carious lesions
Size1: Minimal involvement of dentin just beyond treatment by remineralization alone.
Size2: Moderate involvement of dentin. Following cavity preparation, remaining enamel is sound, well supported by dentin and not likely to fail under normal occlusal load. The remaining tooth structure is sufficiently strong to support the restoration.
Size 3: the cavity is enlarged beyond moderate. The remaining tooth structure is weakened to the extent that cups or incisal edges are split, or are likely to fail or left exposed to occlusal or incisal load. the cavity needs to be further enlarged so that the restoration can be designed to provide support and protection to the remaining tooth structure.
Size4: Extensive caries with bulk loss of tooth structure has already occurred.